PANBIO COVID-19 Ag Rapid Tests
General description
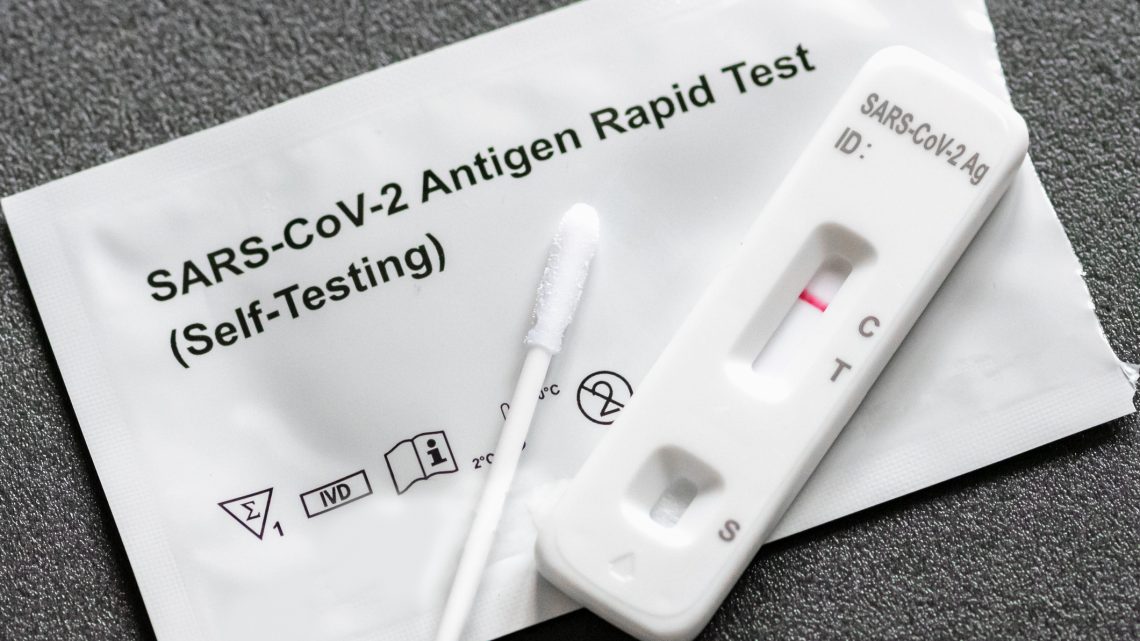
The use of rapid tests has gained wide acceptance as an alternative method for the diagnosis of COVID-19 outside of healthcare settings. Starting in January 2022, all US households are eligible to order four free rapid home antigen tests by mail using covidtests.gov.
These tests differ from molecular tests, such as RT-PCR, because they are designed to detect the presence of viral proteins using simple immunochromatography methods, commonly known as lateral flow assays. Rapid antigen tests target the SARS-CoV-2 nucleocapsid protein, the most abundant protein expressed by the virus. They directly assess the presence of viral proteins, which differentiates them from serological tests, which look for antibodies produced by the host in response to infection. Therefore, rapid antigen tests only assess acute infection, not previous infection or response to vaccination.
Rapid Tests offer a number of advantages over molecular assays. The tests can be implemented outside of hospital laboratories, and many can be carried out by members of the general public. They are relatively inexpensive compared to RT-PCR and easy to interpret. They have a response time of as little as 15 minutes, allowing for testing before entering mass care facilities or other public settings. They are compatible with samples taken from the anterior nares rather than the nasopharynx, making them more convenient for serial testing.
In October 2021, the FDA prioritized making over-the-counter at-home SARS-CoV-2 antigen tests more widely available. This will allow for earlier identification of cases and proactive separation of susceptible hosts. The first test approved through this initiative is the FlowFlex SARS-CoV-2 Rapid Antigen Test from ACON Laboratories, which showed 92% sensitivity relative to PCR when performed on people within a week of symptoms and at asymptomatic people, with a specificity of 100%.

Comparison with RT-PCR
An important difference between rapid antigen tests and RT-PCR is the difference in the analytical sensitivity of the assay. Typically, the sensitivity of antigen tests is 30% to 40% lower than that of RT-PCR, depending on whether the tested subjects were symptomatic or asymptomatic (Cochrane Library, March 2021). However, lower sensitivity has both drawbacks and benefits. The main disadvantage is the risk of false-negative results in people with low viral loads who may be early in their infection and then pass it on to others in the days that follow. In practice, this subpopulation represents only a small fraction of those tested, and the risk can be mitigated through serial testing algorithms.
There is also a slightly high rate of false positives in relation to molecular tests, although the rate depends on the prevalence of the disease and the proportion of people who are symptomatic. For many commonly used rapid antigen tests, the negative predictive value (eg, the probability that someone with a negative test is actually negative for infection) is greater than 98% (Boum, Aug 2021). A major advantage of these assays is the lower probability of detecting residual viral nucleic acid from remote infection in recovered individuals (Mina, November 2020). This reduces the chance that isolation and quarantine precautions and subsequent rounds of testing are unnecessarily initiated.
Rapid antigen tests are subject to the same considerations as molecular tests with respect to factors affecting clinical sensitivity. These include the quality of the sampling and the timing of the test in relation to the onset of infection. They have been found to have reduced performance in the asymptomatic population, which may be related to the lower levels of virus in this group relative to those with symptoms, rather than the characteristics of the tests themselves (Pray, Jan. 2021).
Use cases for rapid antigen tests
Rapid antigen tests for SARS-CoV-2 are in widespread use, but the optimal setting for their implementation remains undefined. Given the lower sensitivities and specificities of rapid tests, programs generally implement confirmatory RT-PCR for positive antigen tests in asymptomatic persons (low pre-test probability) and for negative antigen tests in settings of symptomatic persons and close contacts of positive cases (high pre-test probability). Serial testing is also useful to improve sensitivity and identify infection during the critical period of initial transmission.
A study conducted at two universities in Wisconsin using the Quidel Sofia 2 SARS-CoV-2 antigen assay with middle turbinate swabs reported a sensitivity of 79% in symptomatic and 44% in asymptomatic individuals relative to RT-PCR ( Ford, April 2021; Ore, January 2021). Most false-negative results occurred in people with low virus counts, as inferred by high cycle threshold (Ct) values in RT-PCR. A multicenter descriptive study from Spain evaluating the Abbott PanBio COVID-19 Rapid Ag test reported a sensitivity of 45% in symptomatic children, suggesting reduced performance relative to adults, an important consideration for school-based testing programs.
The extent to which people who are PCR positive/antigen-negative carry the live transmissible viruses is not yet fully understood. Few data exist on changes in the performance of antigen tests in vaccinated individuals, but there is a theoretical risk that receiving a COVID-19 vaccine could result in lower viral loads, which would reduce the sensitivity of the assay. However, recently published data regarding the delta variant suggest that viral loads may be similar in vaccinated and unvaccinated individuals.
